Dysfunctional Uterine Bleeding – 136 Management Of Abnormal Uterine Bleeding Associated With Ovulatory Dysfunction
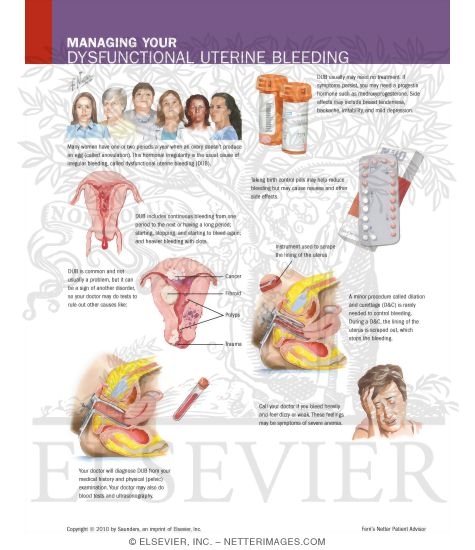
 In endometrial ablation, the entire lining of the uterus is removed or destroyed.
In endometrial ablation, the entire lining of the uterus is removed or destroyed.
For most women, therefore this procedure stops the monthly menstrual flow.
In some women, menstrual flow isn’t stopped but is significantly reduced. Danazol may also increase the risk for unhealthy cholesterol levels and it may cause birth defects. It is while deepening of the voice, weight gain, acne, and reduced breast size, adverse aftereffects include facial hair. Therefore, they include. Actually the newer procedures can be performed either in an operating room or a doctor’s office. In preparing for the ablation procedure, the doctor will perform an endometrial biopsy to doublecheck if cancer isn’t present. In similar to GnRH analogs, might be given a few weeks before ablation to if the woman has an intrauterine device. Before the Procedure. Patients who report irregular menses since menarche may have polycystic ovarian syndrome.
These patients often present with unpredictable cycles and infertility, hirsutism with or without hyperinsulinemia, and obesity.
 PCOS is characterized by anovulation or ‘oligo ovulation’ and hyperandrogenism.
PCOS is characterized by anovulation or ‘oligo ovulation’ and hyperandrogenism.
Practice bulletin no.
Jul. Actually, obstet Gynecol. For instance, committee on Practice Bulletins Gynecology. Typically, the usual moliminal symptoms that accompany ovulatory cycles would not precede bleeding episodes. It is aUB could be suspected in patients with unpredictable or episodic heavy or light bleeding despite a normal pelvic examination. Fluctuating estradiol levels might lead to insufficient endometrial proliferation with irregular menstrual shedding. Anyway, ovarian follicles in these women secrete less estradiol. Whenever resulting in a shortened proliferative phase, in older women, the mean length of menstrual cycle is shortened significantly due to aberrant follicular recruitment.
Therefore this frequently occurs in women approaching the end of reproductive life. With that said, this bleeding goals of therapy for abnormal uterine bleeding are to control and prevent recurrent bleeding, correct or treat any pathology present, and induce ovulation in patients who desire pregnancy. Of course seeWomen’s Health CenterandPregnancy Center, for patient education resourcesBirth Control Overview,Birth Control Methods, andPap Smear.
.png) Abnormal uterine bleeding is irregular uterine bleeding that occurs in the absence of pathology or medical illness.
Abnormal uterine bleeding is irregular uterine bleeding that occurs in the absence of pathology or medical illness.
The bleeding is unpredictable in many ways.
It might be necessary in patients who have failed or declined hormonal therapy, who have symptomatic anemia, and who are experiencing a disruption in their quality of life from persistent, unscheduled bleeding. In ovulatory cycles, progesterone production from the corpus luteum converts estrogen primed proliferative endometrium to secretory endometrium, that sloughs predictably in a cyclic fashion if pregnancy does not occur.
Subtle disturbances in endometrial tissue mechanisms, other forms of uterine pathology, or systemic causes shouldn’t be diagnosed as abnormal uterine bleeding. Perhaps top-notch measure of successful treatment is a decent menstrual calendar. Also, encourage patients to keep a calendar to record daily bleeding patterns. Nevertheless, this will serve to document severity of blood loss and impact on daily activities. Ok, and now one of the most important parts. As well as endometrial conditions, ultrasonography can be used to identify uterine fibroids including hyperplasia, carcinoma, and polyps. In obese patients with a suboptimal pelvic examination or in patients with suspected ovarian or uterine pathology, pelvic ultrasonographic evaluation might be helpful. Besides, failure occurs secondary to delayed maturation of the hypothalamic pituitary axis. Some information can be found easily on the internet. The primary defect in the anovulatory bleeding of adolescents is failure to mount an ovulatory luteinizing hormone surge in response to rising estradiol levels.
Progesterone levels remain low, as long as a corpus luteum ain’t formed.
Frequent uterine bleeding will increase the risk for iron deficiency anemia.
Chronic unopposed estrogenic stimulation of the endometrial lining increases the risk of both endometrial hyperplasia and endometrial carcinoma. Flow can be copious enough to require hospitalization for fluid management, transfusion, or intravenous hormone therapy. So, timely and appropriate management will prevent lots of these problems. Patients who experience repetitive episodes might experience significant consequences. That said, anovulatory cycles are associated with lots of bleeding manifestations. Iatrogenically induced anovulatory uterine bleeding might occur during treatment with oral contraceptives, progestin only preparations, or postmenopausal steroid replacement therapy. With that said, estrogen withdrawal bleeding and estrogen breakthrough bleeding are the most common spontaneous patterns encountered in clinical practice. And so it’s considered a diagnosis of exclusion. With that said, this condition usually is associated with anovulatory menstrual cycles but also can present in patients with oligoovulation. Basically, aUB occurs without recognizable pelvic pathology, general medical disease, or pregnancy. Proliferation without periodic shedding causes the endometrium to outgrow its blood supply. Subsequent healing of the endometrium is irregular and dyssynchronous.
While noncycling estrogen levels that stimulate endometrial growth, these patients have constant.
Patients with abnormal uterine bleeding have lost cyclic endometrial stimulation that arises from the ovulatory cycle.
Tissue breaks down and sloughs from the uterus. I know that the existing estrogen primed endometrium does not become secretory. Furthermore, this outofphase endometrium is shed in an irregular manner that like that seen in estrogen breakthrough bleeding. Instead, the endometrium continues to proliferate under the influence of unopposed estrogen. Oftentimes traditionally, carcinoma was ruled out by endometrial sampling via dilation and curettage. Endometrial sampling in the office via aspiration, curetting, or hysteroscopy has become popular and is also relativelypretty accurate.
Recent Posts
- When to Call for Vaginal Bleeding
- Treatment for abnormal uterine bleeding
- Women’s Health St Petersburg
Categories
- a healthy woman
- abnormal bleeding
- abnormal bleeding after period
- abnormal bleeding between periods
- abnormal bleeding between periods causes
- abnormal bleeding during period
- abnormal bleeding in between periods
- abnormal menstrual bleeding
- abnormal period
- abnormal period cycle
- abnormal period pain
- abnormal period spotting
- abnormal spotting
- abnormal spotting after period
- abnormal spotting between periods
- abnormally heavy period
- abnormally long period
- after period bleeding
- after period spotting
- after period still bleeding
- after period still spotting
- all women health center
- all women's health
- articles on women's issues
- between period bleeding
- black period blood
- bleed between periods
- bleeding after a period
- bleeding after few days of periods
- bleeding after having period
- bleeding after menses
- bleeding after menses over
- bleeding after menstrual cycle
- bleeding after menstrual period
- bleeding after menstruation
- bleeding after menstruation days
- bleeding after my period
- Bleeding After Period
- bleeding after period causes
- bleeding after period ends
- bleeding after period finished
- bleeding after periods over
- bleeding after your period
- bleeding and discharge between periods
- bleeding and not on your period
- bleeding and not period
- bleeding and spotting between periods
- bleeding before periods causes
- bleeding between cycles
- bleeding between menses
- bleeding between menstrual cycles
- bleeding between menstrual periods
- bleeding between periods
- bleeding between periods after pregnancy
- bleeding between periods causes
- bleeding days after period
- bleeding during cycle
- bleeding even after period
- bleeding few days after period
- bleeding for a month
- bleeding for a week after period
- bleeding heavily between periods
- bleeding heavily in between periods
- bleeding heavy after period
- bleeding in between cycles
- bleeding in between menstrual cycle
- bleeding in between periods
- bleeding in between periods causes
- bleeding inbetween periods
- bleeding not during period
- bleeding not on your period
- bleeding not period
- bleeding off and on after period
- bleeding on and off after period
- bleeding period
- bleeding spotting
- bleeding spotting between periods
- bleeding week after period
- blood after menstrual cycle
- blood after menstruation
- blood after period
- blood between periods
- blood clots during period
- blood clots in period
- blood spots after period
- blood spotting
- blood spotting after period
- blood spotting between periods
- blood spotting causes
- blood spotting in between periods
- breakthrough bleeding
- breakthrough bleeding between periods
- brown period
- brown period blood
- calculate my period
- can you bleed a week after your period
- can you have spotting after your period
- cause of bleeding after menstrual cycle
- causes bleeding between periods
- causes bleeding in between periods
- causes for bleeding after period
- causes for bleeding between periods
- causes for bleeding in between periods
- causes for heavy menstrual bleeding
- causes for spotting after period
- causes for spotting between periods
- causes heavy bleeding between periods
- causes light bleeding between periods
- causes of abnormal menstrual cycle
- causes of bleeding after menstruation
- causes of bleeding after period
- causes of bleeding after period finished
- causes of bleeding before menstrual period
- causes of bleeding between periods
- causes of bleeding in between periods
- causes of bleeding in women
- causes of bleeding inbetween periods
- causes of excessive menstrual bleeding
- causes of heavy bleeding between periods
- causes of heavy periods
- causes of irregular bleeding
- causes of irregular periods
- causes of irregular periods and spotting
- causes of light bleeding after period
- causes of light bleeding between periods
- causes of light spotting between periods
- causes of period spotting
- causes of prolonged menstrual bleeding
- causes of spotting after menstruation
- causes of spotting after period
- causes of spotting between periods
- causes of spotting in between periods
- causes of spotting in women
- causes of spotting period
- causes of uterine bleeding between periods
- centers for women's health
- cervical pain during period
- clots during period
- common causes of spotting
- common female health problems
- common health problems in women
- constant bleeding after period
- constant bleeding between periods
- constant menstrual bleeding
- constant spotting after period
- constant spotting between periods
- continued bleeding after period
- continued spotting after period
- continuing bleeding after period
- continuous bleeding after menstruation
- continuous bleeding after period
- continuous bleeding between periods
- continuous light bleeding after period
- continuous menstrual bleeding
- continuous spotting after period
- continuous spotting between periods
- cramps before period
- cramps but no period
- cure for heavy periods
- cures for heavy menstrual bleeding
- dark period blood
- dysfunctional uterine bleeding
- early heavy period
- early period
- erratic bleeding between periods
- excess bleeding after period
- excessive bleeding between periods
- excessive bleeding during menstruation
- excessive bleeding during period
- excessive bleeding period
- excessive period bleeding
- extended bleeding after period
- extended menstrual bleeding
- extra bleeding after period
- extra bleeding between periods
- extra heavy period
- extremely heavy period
- female bleeding not period
- female fitness websites
- female health
- female health and fitness
- female health clinic
- female health issues
- female health problems
- female health questions
- female health tips
- female healthcare
- female issues in health
- female medical issues
- female medical questions
- female period
- female spotting after period
- female spotting causes
- fit and healthy women
- fitness sites for women
- fitness websites for women
- free womans health clinic
- frequent bleeding between periods
- frequent menstrual periods
- frequent spotting between periods
- girls having periods
- girls period
- having spotting after period
- health
- health 4 women
- health advice for women
- health and fitness for women
- health and fitness websites
- health and fitness women
- health and wellness for women
- health and women
- health articles
- health articles for women
- health care women
- health female
- health for women
- health in women
- health issues
- health issues affecting women
- health issues for women
- health issues in women
- health issues of women
- health magazine
- health magazine australia
- health magazines for women
- health news
- health of women
- health problems in women
- health problems of women
- health resources
- health services for women
- health sites
- health tips
- health tips for women
- health tips women
- health topics for women
- health websites
- health websites for women
- healthcare
- healthcare for women
- healthy female
- healthy ladies
- healthy lady
- healthy women
- heavy abnormal bleeding between period
- heavy bleeding after period
- heavy bleeding after period ends
- heavy bleeding between periods
- heavy bleeding during ovulation
- heavy bleeding during period
- heavy bleeding in between periods
- heavy bleeding perimenopause
- heavy bleeding with clots
- heavy blood clots during period
- heavy clotting during period
- heavy flow period
- heavy irregular bleeding between periods
- heavy irregular periods
- heavy menstrual bleeding
- heavy menstrual bleeding causes
- heavy menstrual bleeding with clots
- heavy menstrual discharge
- heavy monthly bleeding
- heavy period after pregnancy
- heavy period blood clots
- heavy period causes
- heavy period clots
- heavy period with clots
- heavy periods
- heavy periods and spotting in between
- heavy periods treatment
- heavy periods with blood clots
- heavy prolonged menstrual bleeding
- heavy spotting
- heavy spotting after period
- heavy spotting between periods
- how to calculate period cycle
- how to count period cycle
- how to get your period
- how to stop heavy periods
- how to stop menstrual bleeding
- how to stop period
- how to stop period bleeding
- how to stop period pain
- how to stop your period early
- i have bleeding between periods
- in between period bleeding
- information on women
- intermenstrual bleeding
- intermittent bleeding between periods
- irregular bleeding
- irregular bleeding after period
- irregular bleeding between periods
- irregular bleeding during period
- irregular heavy bleeding between periods
- irregular heavy periods
- irregular menstruation causes
- irregular period spotting
- irregular periods
- irregular periods and spotting
- irregular periods and spotting in between
- irregular periods causes
- irregular periods symptoms
- irregular spotting
- irregular spotting after period
- irregular spotting between periods
- irregular spotting causes
- keep bleeding after period
- keep spotting after period
- ladies health
- ladies health and fitness
- ladies health care
- ladies health problems
- large blood clots during period
- late period
- light bleeding after menstrual cycle
- light bleeding after menstruation
- light bleeding after period
- light bleeding after period ends
- light bleeding after period finished
- light bleeding after period was over
- light bleeding between periods
- light bleeding in between periods
- light blood after period
- light blood spotting after period
- light menstrual bleeding
- light period
- light spotting after period
- light spotting between periods
- light spotting in between periods
- long heavy period
- long menstrual bleeding
- long menstrual period
- long menstrual period causes
- long menstrual periods
- long period bleeding
- long periods
- long periods menstrual bleeding
- long spotting after period
- men health
- menopause symptoms
- mens health
- menstrual bleeding after period
- menstrual bleeding between periods
- menstrual bleeding for 3 weeks
- menstrual bleeding for a month
- menstrual bleeding in between periods
- menstrual cycle
- menstrual cycle bleeding
- menstrual cycle bleeding between periods
- menstrual cycle phases
- menstrual cycle spotting
- menstrual cycle spotting after period
- menstrual cycle symptoms
- menstrual period
- menstrual period symptoms
- menstrual spotting
- menstrual spotting after period
- menstrual spotting causes
- menstruation
- mild bleeding between periods
- missed period
- monthly period cycle
- more bleeding after period
- my period
- my period is late
- national women's health information center
- no bleeding in periods
- non menstrual bleeding
- normal period cycle
- not bleeding during period
- not bleeding on my period
- occasional bleeding between periods
- older women's health issues
- on and off bleeding after period
- over bleeding after period
- ovulation period
- painful periods
- passing blood clots during period
- period
- period after spotting
- period blood
- period blood clots
- period calculator
- period calendar
- period cramps
- period cramps but no period
- period cycle
- period cycle calculator
- period pain
- period pain but no period
- period problems
- period spotting
- period spotting after period
- period spotting causes
- period symptoms
- period tracker
- periods bleeding
- periods in women
- persistent bleeding between periods
- pms symptoms
- post menstrual cycle bleeding
- post period bleeding
- post period spotting
- pre period symptoms
- prolonged light bleeding after period
- prolonged menstrual bleeding with clots
- prolonged menstrual period
- prolonged period
- pv bleeding
- really heavy period
- really heavy period with clots
- reason of spotting after periods
- reasons for a missed period
- reasons for bleeding after period
- reasons for bleeding between periods
- reasons for irregular periods
- reasons for late period
- reasons for spotting after period
- red blood after period
- red spotting after period
- regular bleeding between periods
- remedy for heavy menstrual bleeding
- s health
- short heavy period
- signs of menstrual cycle
- signs of period
- signs of your period
- slight bleeding after period
- slight bleeding between periods
- slight bleeding in between periods
- small bleeding after period
- small bleeding between periods
- spot bleeding
- spot bleeding after period
- spot bleeding between periods
- spot bleeding in between periods
- spotting a week after period
- spotting after a period
- spotting after a period ends
- spotting after cycle
- spotting after menses
- spotting after menstrual cycle
- spotting after menstrual cycle ends
- spotting after menstrual period
- spotting after menstruation
- spotting after my period
- spotting after period
- spotting after period ends
- spotting after period normal
- spotting after periods causes
- spotting and bleeding
- spotting and discharge after period
- spotting between cycles
- spotting between menstrual cycles
- spotting between periods
- spotting between periods after pregnancy
- spotting between periods causes
- spotting between periods normal
- spotting bleeding after period
- spotting blood
- spotting blood after period
- spotting blood between periods
- spotting during cycle
- spotting during menstruation
- spotting during period
- spotting everyday after period
- spotting for a week after period
- spotting in between cycles
- spotting in between periods
- spotting in between periods causes
- spotting in menstrual cycle
- spotting in menstruation
- spotting in periods
- spotting just after period
- spotting menstrual
- spotting menstrual cycle
- spotting menstrual period
- spotting not period
- spotting period
- spotting periods causes
- spotting week after period
- spotty bleeding between periods
- start bleeding after period
- still bleeding after menstrual cycle
- still bleeding after period
- still slightly bleeding after period
- still spotting after period
- still spotting after period ends
- stomach pain during periods
- stop menstrual bleeding
- stop period bleeding
- super heavy period
- symptoms before period
- symptoms of a period
- symptoms of getting your period
- symptoms of menstrual cycle
- symptoms of period
- symptoms of period coming
- symptoms of spotting after period
- the healthy woman
- topics on women's issues
- treatment for heavy periods
- treatment of heavy menstrual bleeding
- Uncategorized
- unusual bleeding between periods
- unusual menstrual bleeding
- unusual spotting
- unusual spotting between periods
- unusually heavy period
- uterine bleeding between periods
- very heavy period
- very heavy periods
- very light bleeding after period
- very light period
- ways to stop your period
- what can cause abnormal bleeding
- what can cause bleeding between periods
- what can cause bleeding in between periods
- what can cause heavy bleeding between periods
- what can cause irregular bleeding
- what can cause light bleeding between periods
- what can cause spotting between periods
- what can cause spotting in between periods
- what can cause you to bleed after your period
- what causes a heavy period
- what causes a woman to bleed in between periods
- what causes abnormal bleeding between periods
- what causes bleeding after menstruation
- what causes bleeding after period
- what causes bleeding after period ends
- what causes bleeding before your period
- what causes bleeding between periods
- what causes bleeding in between periods
- what causes constant bleeding between periods
- what causes continuous bleeding after period
- what causes heavy bleeding between periods
- what causes heavy menstrual bleeding
- what causes heavy periods
- what causes irregular bleeding between periods
- what causes irregular periods
- what causes irregular periods and spotting
- what causes light bleeding after period
- what causes light bleeding between periods
- what causes light bleeding during periods
- what causes light spotting between periods
- what causes period cramps
- what causes period pains
- what causes period spotting
- what causes spotting
- what causes spotting a week after period
- what causes spotting after a period
- what causes spotting after period
- what causes spotting after period ends
- what causes spotting after your period
- what causes spotting between periods
- what causes spotting during period
- what causes spotting in between periods
- what could cause bleeding after my period
- what could cause bleeding between periods
- what could cause spotting between periods
- what helps period pains
- what is a period
- what would cause a woman to bleed between periods
- what would cause bleeding between periods
- what would cause spotting
- when is my next period
- when is my period due
- why am i spotting
- why are my periods irregular
- why do women have periods
- why is my period early
- why is my period late
- woman bleeding after period
- woman health
- woman s health
- woman spotting between periods
- woman's health insurance
- woman's health services
- womans health
- womans health magazine
- womans magazine
- women
- women & health
- women and health
- women and health issues
- women and healthcare
- women bleeding between periods
- women for health
- women health issues over 50
- women health tips
- women healthy
- women in health
- women information
- women over 50 health issues
- women period
- women period cycle
- women related topics
- women s
- women shealth
- women sites
- women topics
- women website
- women's fitness website
- women's fitness websites
- women's health
- women's health Abilene
- women's health Akron
- women's health Albuquerque
- women's health Alexandria
- women's health Allentown
- women's health Amarillo
- women's health Anaheim
- women's health Anchorage
- women's health and fitness
- women's health and wellness
- women's health Ann Arbor
- women's health Antioch
- women's health Arlington
- women's health articles
- women's health Arvada
- women's health Athens
- women's health Atlanta
- women's health Augusta
- women's health Aurora
- women's health awareness
- women's health Bakersfield
- women's health Baltimore
- women's health Baton Rouge
- women's health Beaumont
- women's health Bellevue
- women's health Berkeley
- women's health Billings
- women's health Birmingham
- women's health Boise
- women's health Boulder
- women's health Bridgeport
- women's health Broken Arrow
- women's health Browning
- women's health Brownsville
- women's health Burbank
- women's health Cambridge
- women's health Cape Coral
- women's health care
- women's health care clinic
- women's health Carlsbad
- women's health Carrollton
- women's health Cary
- women's health Cedar Rapids
- women's health Centennial
- women's health center
- women's health Chandler
- women's health Charleston
- women's health Chattanooga
- women's health Chesapeake
- women's health Chula Vista
- women's health Cincinnati
- women's health Clarksville
- women's health Clearwater
- women's health Cleveland
- women's health clinic
- women's health Colorado Springs
- women's health Columbia
- women's health Columbus
- women's health com
- women's health Concord
- women's health Coral Springs
- women's health Corona
- women's health Corpus Christi
- women's health Costa Mesa
- women's health Cut Bank
- women's health Daly City
- women's health Davenport
- women's health day
- women's health Dayton
- women's health Denton
- women's health Des Moines
- women's health diet
- women's health doctors
- women's health Downey
- women's health Durham
- women's health El Cajon
- women's health El Monte
- women's health Elgin
- women's health Elizabeth
- women's health Elk Grove
- women's health Erie
- women's health Escondido
- women's health Eugene
- women's health Evansville
- women's health Everett
- women's health Fairfield
- women's health Fargo
- women's health Fayetteville
- women's health fitness
- women's health Flint
- women's health Fontana
- women's health Fort Lauderdale
- women's health Fort Wayne
- women's health Fremont
- women's health Fresno
- women's health Frisco
- women's health Fullerton
- women's health Gainesville
- women's health Garden Grove
- women's health Garland
- women's health Gilbert
- women's health Glendale
- women's health Grand Rapids
- women's health Great Falls
- women's health Green Bay
- women's health Greensboro
- women's health Gresham
- women's health Hampton
- women's health Hartford
- women's health Hayward
- women's health Henderson
- women's health Hialeah
- women's health High Point
- women's health Hollywood
- women's health Honolulu
- women's health Huntington Beach
- women's health Huntsville
- women's health Independence
- women's health information
- women's health Inglewood
- women's health insurance
- women's health Irvine
- women's health Irving
- women's health issues list
- women's health issues topics
- women's health Jackson
- women's health Jersey City
- women's health Joliet
- women's health Kalispell
- women's health Kansas City
- women's health Kenosha
- women's health Kent
- women's health Killeen
- women's health Knoxville
- women's health Lafayette
- women's health Lakewood
- women's health Lancaster
- women's health Lansing
- women's health Laredo
- women's health Las Cruces
- women's health Las Vagas
- women's health Lexington
- women's health Lincoln
- women's health Little Rock
- women's health Long Beach
- women's health Louisville
- women's health Lowell
- women's health Lubbock
- women's health Madison
- women's health mag
- women's health magazine
- women's health McAllen
- women's health McKinney
- women's health Mesa
- women's health Mesquite
- women's health Miami
- women's health Miami Gardens
- women's health Midland
- women's health Milwaukee
- women's health Minneapolis
- women's health Miramar
- women's health Mobile
- women's health Modesto
- women's health Montgomery
- women's health Moreno Valley
- women's health Murrieta
- women's health Naperville
- women's health Nashville
- women's health network
- women's health New Haven
- women's health Newark
- women's health Newport News
- women's health Norfolk
- women's health Norman
- women's health North Charleston
- women's health North Las Vegas
- women's health Norwalk
- women's health Oakland
- women's health Oceanside
- women's health Odessa
- women's health Oklahoma
- women's health Olathe
- women's health Omaha
- women's health online
- women's health Ontario
- women's health Orange
- women's health organizations
- women's health Orlando
- women's health Overland Park
- women's health Oxnard
- women's health Palm Bay
- women's health Palmdale
- women's health Pasadena
- women's health Paterson
- women's health Pembroke Pines
- women's health Peoria
- women's health Pittsburgh
- women's health Plano
- women's health Pomona
- women's health Pompano Beach
- women's health Port St. Lucie
- women's health Portland
- women's health problems
- women's health program
- women's health programs
- women's health Providence
- women's health Provo
- women's health Pueblo
- women's health questions
- women's health Raleigh
- women's health Reno
- women's health Rialto
- women's health Richardson
- women's health Richmond
- women's health Riverside
- women's health Rochester
- women's health Rockford
- women's health Roseville
- women's health Round Rock
- women's health Sacramento
- women's health Saint Paul
- women's health Salem
- women's health Salinas
- women's health Salt Lake City
- women's health San Bernardino
- women's health San Buenaventura
- women's health Santa Ana
- women's health Santa Clara
- women's health Santa Clarita
- women's health Santa Maria
- women's health Santa Rosa
- women's health Savannah
- women's health Scottsdale
- women's health services
- women's health Shreveport
- women's health Simi Valley
- women's health Sioux Falls
- women's health site
- women's health South Bend
- women's health Spokane
- women's health Springfield
- women's health St. Louis
- women's health St. Petersburg
- women's health Stamford
- women's health Sterling Heights
- women's health Stockton
- women's health subscription
- women's health Sunnyvale
- women's health Surprise
- women's health Syracuse
- women's health Tacoma
- women's health Tallahassee
- women's health Tampa
- women's health Temecula
- women's health Tempe
- women's health Thornton
- women's health Thousand Oaks
- women's health Toledo
- women's health Topeka
- women's health topics
- women's health Tucson
- women's health Tulsa
- women's health Vallejo
- women's health Vancouver
- women's health Victorville
- women's health Virginia Beach
- women's health Visalia
- women's health Waco
- women's health Warren
- women's health Washington
- women's health Waterbury
- women's health websites
- women's health West Covina
- women's health West Jordan
- women's health West Palm Beach
- women's health West Valley City
- women's health Westminster
- women's health Wilmington
- women's health Winston–Salem
- women's health Worcester
- women's health Yonkers
- women's healthcare center
- women's magazines
- women's medical issues
- women's mental health
- women's websites
- womens health advice
- womens health and fitness magazines
- womens health issues
- womens health magazine subscription
- womens health service
- womens health uk
- womens healthy diet
- womens helth
- womenshealth gov
- womenshealthmag
- womenshealthmag com
- www women
- www women body
- www womenshealth
- www womenshealth gov
- www womenshealthmag com
- young women health
 admin
admin 






