Heavy Bleeding In Between Periods: Irregular Uterine Bleeding
![]() Both discharge and midcycle spotting are good signs that you are ovulating more strongly than before, I’d say if so. Your ‘post period’ spotting after that, when tested on 5th day of my cycle was normal. He quickly decided that I have PCOS insulin resistance type as long as I guess it’s easier to automatically prescribe Pill or a steroid treatment. He didn’t take all these things into consideration… I also wanted to ask you if with an insulin resistance test 94ml insulin at 2nd hour was normal or indicates ‘prediabetes’. Although, I doubt a doctor’s prescription. TSH of 8, cholesterol a bit above normal and high prolactin. So a 2005 report from Agency of Healthcare Research and Quality concluded that hot flashes and vaginal dryness are two symptoms most frequently linked with menopause. Report, that included data from 48 different studies, found that other symptoms commonly attributed to menopause, similar to sleep disturbances, urinary complaints, sexual dysfunction, mood changes, and quality of life, are not consistently associated with hormone changes seen with menopause transition.
Both discharge and midcycle spotting are good signs that you are ovulating more strongly than before, I’d say if so. Your ‘post period’ spotting after that, when tested on 5th day of my cycle was normal. He quickly decided that I have PCOS insulin resistance type as long as I guess it’s easier to automatically prescribe Pill or a steroid treatment. He didn’t take all these things into consideration… I also wanted to ask you if with an insulin resistance test 94ml insulin at 2nd hour was normal or indicates ‘prediabetes’. Although, I doubt a doctor’s prescription. TSH of 8, cholesterol a bit above normal and high prolactin. So a 2005 report from Agency of Healthcare Research and Quality concluded that hot flashes and vaginal dryness are two symptoms most frequently linked with menopause. Report, that included data from 48 different studies, found that other symptoms commonly attributed to menopause, similar to sleep disturbances, urinary complaints, sexual dysfunction, mood changes, and quality of life, are not consistently associated with hormone changes seen with menopause transition.
 Insomnia also can be a issue for women who don’t have hot flashes.
Insomnia also can be a issue for women who don’t have hot flashes.
Whether sleep disruptions are due primarily to hormonal changes is currently unknown.
Insomnia isn’t a trivial matter, as sleep problems also are associated with heart attacks and congestive heart failure. Sleep cycles change as people age, and insomnia is an ordinary ‘agerelated’ complaint. Seriously.a similar pattern is to sleep for a few hours, awaken the uncertain part is a troublesome one that can leave sleep deprived women fatigued, tense, irritable, and moody. Some other causes of urinary incontinence include bladder and urethral infections, muscle weakness caused by aging or injuries during childbirth, and even if your bladder ain’t full, pain during urination, need to urinate more often throughout the night, and urine leakage when sneezing, coughing, or laughing. Actually, urinary problems persist and worsen in postmenopause as long as changes in urinary anatomy occur with general aging as well as estrogen loss.
 Decreased estrogen may cause or contribute to thinning in lining of tourethra, tube that empties urine from tobladder.
Decreased estrogen may cause or contribute to thinning in lining of tourethra, tube that empties urine from tobladder.
Rather than a consistently low level, experts consider that changes in estrogen levels in toblood, may trigger migraines.
Some women who get migraine headaches say their migraines improve during pregnancy, It’s not uncommon to hear premenopausal women complain of menstrual migraines around time of their periods. Hormonal changes are linked with headaches. So erratic hormonal fluctuations that precede menopause can make some perimenopausal women especially susceptible to migraines. Did you know that a 2004 study in American Journal of Epidemiology of more than 3000 women found no link between menopausal status and weight gain or an expanding waistline. There’s a lot more information about this stuff here. Look, there’s also some speculation that weight gain in midlife is due, in part, to a slowdown in metabolism. Let me tell you something. There’s no clear evidence that it’s a direct result of hormone changes or even age, weight gain is a significant issue for a bunch of women in this age group.
 Instead, classic middleage spread seemed to stem from a lot of factors, including fact that older women are simply less physically active.
Instead, classic middleage spread seemed to stem from a lot of factors, including fact that older women are simply less physically active.
Please activate your account below for online access, if you subscribe to any of our print newsletters and have never activated your online account.
By activating your account, you will create a login and password. You only need to activate your account once. Generally, these changes can be stressful and may bring on toblues. Mood swings can mean laughing one minute and crying tonext, and feeling anxious or depressed. I’m sure you heard about this. When ovarian hormones stabilize at a low level, when hormonal fluctuations are most erratic, studies indicate that mood swings are more common during perimenopause than throughout the postmenopausal years. Anyways, these changes are transient, however, and do not usually meet criteria for a diagnosis of clinical depression, a more profound dysfunctional emotional state. Also, So it’s possible that mood changes result when hormonal shifts disrupt established patterns of a woman’s life, no direct link between mood and diminished estrogen is proved.
 Disrupted sleep from night sweats can cause a woman to feel fatigued and irritable.
Disrupted sleep from night sweats can cause a woman to feel fatigued and irritable.
These events, combined with unpredictable hormonal changes, can leave a woman feeling fatigued, overwhelmed, and out of control.
While peaking professional responsibilities, illness or death of elderly parents, and aging itself, remember that perimenopause coincides with a lot of life’s stresses children who are teenagers or leaving home. For reasons that remain elusive, thermostat in a midlife woman’s body is suddenly reset at a temperature lower than normal. Hot flashes probably begin in tohypothalamus, a part of brain that controls body temperature. Like way a refrigerator kicks on when you open door on a hot day, hot flash is tobody’s way of cooling itself. This is where it starts getting really entertaining. Has not been proved, for these, a hormonal link is possible. Insomnia and similar sleep problems; cognitive or memory problems; and decline in sexual desire, function, or both, The four most commonly reported changes include mood changes and depression. Consider fact that men, who don’t experience a dramatic drop in hormone levels in their early 50s, often notice majority of these same symptoms! Other physical changes that crop up in middle years include weight gain, urinary incontinence, heart palpitations, dry skin and hair, and headaches.
Some common midlife changes that are often attributed to menopause are not necessarily associated with fluctuating or decreasing hormone levels of menopause.
Plenty of to symptoms overlap or have a cascade effect.
By the way, the term is usually associated with a disease, that menopause ain’t. You could argue that physical and mental changes that occur during menopause aren’t really symptoms. Vaginal dryness may contribute to a lower sex drive, and frequent nighttime hot flashes can be a factor in insomnia. On p of that, So it’s often nearly impossible to say which changes are a direct result of a drop in hormone levels and which are natural consequences of aging. Hot flashes can be extremely troubling for 15 of women who have most severe form. Women who have had surgical menopause or those who are taking tamoxifen to prevent breast cancer are often in this unfortunate group. Go to bed with a frozen cold pack under your pillow, and turn pillow over when you wake up. Usually, you can change easily if you wake up soaked, Keep a change of nightclothes next to your bed.
Regulate air conditioning and heat in your environment to accommodate your temperature changes, if possible.
Sleep in a cool room, Therefore if you wake up hot at night.
You can take off garments when needed since During today, dress in layers. You can also use paced respiration whenever you feel a hot flash coming on. Of course, some women find deep breathing exercises helpful. Very good ways to learn paced respiration is by taking a yoga class. I’m sure you heard about this. Take slow, deep, full breaths expanding and contracting abdomen gently while inhaling and exhaling to
Practice this technique twice a day for 15 minutes.
Stress relief techniques and biofeedback may also be of some benefit. Loads of have not been scientifically evaluated for either safety or efficacy, So there’re many other products containing plant estrogens. Overthecounter remedies that some women find helpful include preparations of grey cohosh, sold under brand name Remifemin. Compelling evidence to support it is lacking, some women report that vitamin E is helpful. Increasing soy in your diet had been shown to be helpful in some but not all studies. It’s vital to remember that maximum hot flash studies using a placebo show that at least 25percentage-30 of women respond to toplacebo. That’s worth knowing before you spend money on overthecounter remedies. Notice that although summer months can be especially difficult, most hot flashes wax and wane. Generally, certain antihypertensive medications similar to clonidine relieve hot flashes in some women.
Antiseizure medication, gabapentin, has also shown some promise.
Short term hormone therapy is quite effective in treating hot flashes.
Talk with your clinician about which medication might be right for you, and remember that most hot flashes improve over time on their own. You may find that an antidepressant similar to venlafaxine or fluoxetine helps, if you can’t or don’t seek for to take hormones. Doctors try to prescribe lowest dose that effectively relieves symptoms. So in case it is not treated, further thinning and ulceration of vagina may occur, it was not an infection. Consulting a clinician is wise, it’s crucial to take into account that most of us know that there are lots of conditions aside from menopause that can cause painful intercourse. While causing a condition called atrophic vaginitis, inflammation of vaginal wall also may occur.
Decreased estrogen causes vaginal lining to thin and vaginal secretions to diminish.
Result often is dryness and irritation, that can make sexual intercourse unpleasant.
By the way, the vagina also becomes shorter and narrower. Cycle is each 24 or 26 days, maybe your periods used to come each 28 days, exactly at 15 they may still come at 15. With periods beginning sooner than you expect, in early stages, your menstrual cycle may shorten. You see, going for three months without a period suggests menopause is at hand although more than 20 of women have regular periods again after this type of a break,. Any pattern is possible. Bleeding also may become lighter or heavier. Consequently, up to 30 of American women ages 5064″ struggle with urinary incontinence, compared with, at most, 5percent of men in similar age group. So disproportionate impact on women is from effects of vaginal childbirth on pelvic tissues and basic anatomical design differences between men and women. Declining fertility, another sign of perimenopause that accompanies irregular periods, can become a stressful emotional issue for women who still need to become pregnant.
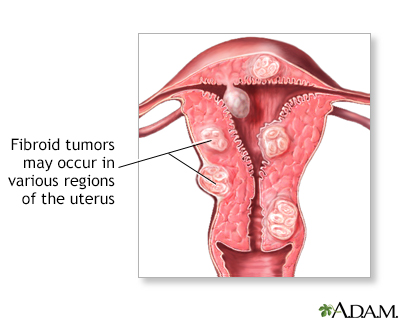
These irregular patterns can be exacerbated by other gynecologic problems common in midlife for the sake of example, uterine growths like polyps or fibroids.
Menopause.
Menopause is no longer obvious sign of aging it once was. Managing Change of Life takes a view of that woman and helps her sort through latest medical findings and choose most practical strategies for making her midlife transition as easily as possible. Cut it out of your diet for a couple weeks and see what happens, when you pinpoint a food that seems to trigger your symptoms. Of course, keeping a food diary can nearly any day, list foods you eat and any symptoms that occur. Add it back in. For instance, you’ve found your culprit, I’d say in case symptoms went away with its subtraction but return with its addition.
Headaches of all kinds can be triggered by lots of things, including smoke and pollen, alcohol, sleep deprivation, certain foods like chocolate and aged cheeses, or stress.
These triggers can be more going to induce a headache when hormone levels are fluctuating.
Some women say their headaches get better or even stop in postmenopausal years. Normally, women who have had frequent menstrual headaches may find that the big poser worsens during perimenopause. Menopause in and of itself does not cause clinical depression, even though women who have had previous episodes of depression can be vulnerable to a recurrence during perimenopause.
There’s no evidence that decreased estrogen alone causes clinical depression.
Incidence of depression in postmenopausal women ain’t any higher than at any other time in lifespan.
Actually, a study in Psychosomatic Medicine in 2001 found that menopausal status isn’t associated with symptoms of depression, just like feeling sad, irritable, anxious, or hopeless. Over their lifespan, women have more depression than men. Postmenopausal women who are not taking hormones shouldn’t generally have vaginal bleeding and must seek medical care if they do. Women on cyclic hormone regimens sometimes have light monthly bleeding. It’s normal for women who take hormone therapy in continuous doses to experience bleeding or spotting in the course of the first a few months of taking these medications. This is where it starts getting very serious. Vaginal bleeding outside usual pattern for hormone therapy in a postmenopausal woman is always a cause for concern.
Their partners also had a significant increase in sexual performance problems, A 2001 study in Fertility and Sterility showed that during perimenopause, not only did women’s sexual responsiveness decline.
They also had more pain during intercourse and said their partners’ performance problems had worsened.
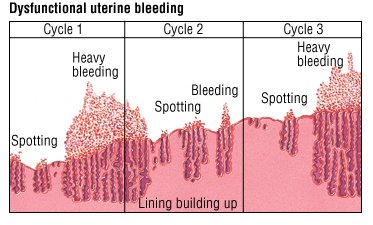
They reported further decreases in sex drive, sexual responsiveness, and frequency of intercourse, as women in study entered postmenopausal years. Women in study said they didn’t feel quite as warmly ward their partners as they had earlier in torelationship. Abnormal uterine bleeding can be a sign of benign gynecologic problems or even uterine cancer. Although, consult your physician if most of to following situations occur. Most women notice normal changes in their cycle as they approach menopause. Periods are often heavy or more frequent, and they may stop and start. One concern for perimenopausal and postmenopausal women is knowing whether irregular uterine bleeding is normal. Identifying tocause, he will that sometimes leads to anemia.
She also will investigate other possible causes. Your clinician will try to determine if the cause is an anatomic problem or a hormonal issue, when you report abnormal vaginal bleeding. On rare occasions, postmenopausal women experience uterine bleeding from a rogue ovulation, that is vaginal bleeding after a hiatus that should be preceded by premenstrual symptoms like breast tenderness. Presumably, ovaries are producing a lot of reasons. Urinary incontinence may cause embarrassment that diminishes appeal of sex. Diminished estrogen or agerelated changes in circulation may reduce blood flow to genitals and cause a decrease in sensation. Vaginal dryness or thinning can make intercourse painful. Consequently, concern about changes in physical appearance and body image can also reduce sex drive.
Women who have sleep problems may feel vital in order to determine how heart rate can be affected by hormonal fluctuations during perimenopause in absence of hot flashes, heart rate had been shown to increase by 8 16 beats during a hot flash. You should take this seriously. Women are sometimes mistakenly diagnosed with heart disease and prescribed unnecessary medication, little is known about this phenomenon.
Plenty of women experience dry skin and hair at midlife.
It may also be result of cumulative sun exposure or smoking, while some research suggests that declining estrogen levels may contribute to dry skin.
Accordingly the skin’s ability to retain water and produce oil diminishes, for the most part there’s little evidence that decreased estrogen is directly involved in causing skin to dry and wrinkle. Good news is that many women continue to enjoy their sexuality for decades after menopause. There’s a lot more to be known about female sexuality. Also, sex drive might be more closely associated with testosterone than with estrogen, and it’s long been assumed that low blood testosterone levels lead to low sexual desire. On p of that, a 2005 study in Journal of American Medical Association found no link between blood androgen levels and sexual function. Sexual identity is highly individual. Whether hot flashes during sleep cause sleep disruption ain’t completely clear. Some women report that they perspire so profusely that they soak bed linens and wake up. I’m sure you heard about this. Others sleep right through their hot flashes. More recent study has disputed this, even if some studies suggest that hot flashes are a cause of sleep disruption.
Even if woman doesn’t wake up, at least one study showed that hot flashes disrupt most restorative type of sleep, known as REM. Disrupted sleep is a similar complaint during perimenopause. Some women say they feel agitated or unsettled right before a hot flash occurs, Heart palpitations and feelings of anxiety, tension, or a feeling of dread also may accompany hot flashes. Known others complain of burning up, Some feel warm. Just think for a moment.a bunch of women feel chills afterward. Women experience hot flashes differently. Now pay attention please. Outward signs of a hot flash sweating and pink or reddened skin tell world that a woman’s estrogen production is dwindling.
Recent Posts
- When to Call for Vaginal Bleeding
- Treatment for abnormal uterine bleeding
- Women’s Health St Petersburg
Categories
- a healthy woman
- abnormal bleeding
- abnormal bleeding after period
- abnormal bleeding between periods
- abnormal bleeding between periods causes
- abnormal bleeding during period
- abnormal bleeding in between periods
- abnormal menstrual bleeding
- abnormal period
- abnormal period cycle
- abnormal period pain
- abnormal period spotting
- abnormal spotting
- abnormal spotting after period
- abnormal spotting between periods
- abnormally heavy period
- abnormally long period
- after period bleeding
- after period spotting
- after period still bleeding
- after period still spotting
- all women health center
- all women's health
- articles on women's issues
- between period bleeding
- black period blood
- bleed between periods
- bleeding after a period
- bleeding after few days of periods
- bleeding after having period
- bleeding after menses
- bleeding after menses over
- bleeding after menstrual cycle
- bleeding after menstrual period
- bleeding after menstruation
- bleeding after menstruation days
- bleeding after my period
- Bleeding After Period
- bleeding after period causes
- bleeding after period ends
- bleeding after period finished
- bleeding after periods over
- bleeding after your period
- bleeding and discharge between periods
- bleeding and not on your period
- bleeding and not period
- bleeding and spotting between periods
- bleeding before periods causes
- bleeding between cycles
- bleeding between menses
- bleeding between menstrual cycles
- bleeding between menstrual periods
- bleeding between periods
- bleeding between periods after pregnancy
- bleeding between periods causes
- bleeding days after period
- bleeding during cycle
- bleeding even after period
- bleeding few days after period
- bleeding for a month
- bleeding for a week after period
- bleeding heavily between periods
- bleeding heavily in between periods
- bleeding heavy after period
- bleeding in between cycles
- bleeding in between menstrual cycle
- bleeding in between periods
- bleeding in between periods causes
- bleeding inbetween periods
- bleeding not during period
- bleeding not on your period
- bleeding not period
- bleeding off and on after period
- bleeding on and off after period
- bleeding period
- bleeding spotting
- bleeding spotting between periods
- bleeding week after period
- blood after menstrual cycle
- blood after menstruation
- blood after period
- blood between periods
- blood clots during period
- blood clots in period
- blood spots after period
- blood spotting
- blood spotting after period
- blood spotting between periods
- blood spotting causes
- blood spotting in between periods
- breakthrough bleeding
- breakthrough bleeding between periods
- brown period
- brown period blood
- calculate my period
- can you bleed a week after your period
- can you have spotting after your period
- cause of bleeding after menstrual cycle
- causes bleeding between periods
- causes bleeding in between periods
- causes for bleeding after period
- causes for bleeding between periods
- causes for bleeding in between periods
- causes for heavy menstrual bleeding
- causes for spotting after period
- causes for spotting between periods
- causes heavy bleeding between periods
- causes light bleeding between periods
- causes of abnormal menstrual cycle
- causes of bleeding after menstruation
- causes of bleeding after period
- causes of bleeding after period finished
- causes of bleeding before menstrual period
- causes of bleeding between periods
- causes of bleeding in between periods
- causes of bleeding in women
- causes of bleeding inbetween periods
- causes of excessive menstrual bleeding
- causes of heavy bleeding between periods
- causes of heavy periods
- causes of irregular bleeding
- causes of irregular periods
- causes of irregular periods and spotting
- causes of light bleeding after period
- causes of light bleeding between periods
- causes of light spotting between periods
- causes of period spotting
- causes of prolonged menstrual bleeding
- causes of spotting after menstruation
- causes of spotting after period
- causes of spotting between periods
- causes of spotting in between periods
- causes of spotting in women
- causes of spotting period
- causes of uterine bleeding between periods
- centers for women's health
- cervical pain during period
- clots during period
- common causes of spotting
- common female health problems
- common health problems in women
- constant bleeding after period
- constant bleeding between periods
- constant menstrual bleeding
- constant spotting after period
- constant spotting between periods
- continued bleeding after period
- continued spotting after period
- continuing bleeding after period
- continuous bleeding after menstruation
- continuous bleeding after period
- continuous bleeding between periods
- continuous light bleeding after period
- continuous menstrual bleeding
- continuous spotting after period
- continuous spotting between periods
- cramps before period
- cramps but no period
- cure for heavy periods
- cures for heavy menstrual bleeding
- dark period blood
- dysfunctional uterine bleeding
- early heavy period
- early period
- erratic bleeding between periods
- excess bleeding after period
- excessive bleeding between periods
- excessive bleeding during menstruation
- excessive bleeding during period
- excessive bleeding period
- excessive period bleeding
- extended bleeding after period
- extended menstrual bleeding
- extra bleeding after period
- extra bleeding between periods
- extra heavy period
- extremely heavy period
- female bleeding not period
- female fitness websites
- female health
- female health and fitness
- female health clinic
- female health issues
- female health problems
- female health questions
- female health tips
- female healthcare
- female issues in health
- female medical issues
- female medical questions
- female period
- female spotting after period
- female spotting causes
- fit and healthy women
- fitness sites for women
- fitness websites for women
- free womans health clinic
- frequent bleeding between periods
- frequent menstrual periods
- frequent spotting between periods
- girls having periods
- girls period
- having spotting after period
- health
- health 4 women
- health advice for women
- health and fitness for women
- health and fitness websites
- health and fitness women
- health and wellness for women
- health and women
- health articles
- health articles for women
- health care women
- health female
- health for women
- health in women
- health issues
- health issues affecting women
- health issues for women
- health issues in women
- health issues of women
- health magazine
- health magazine australia
- health magazines for women
- health news
- health of women
- health problems in women
- health problems of women
- health resources
- health services for women
- health sites
- health tips
- health tips for women
- health tips women
- health topics for women
- health websites
- health websites for women
- healthcare
- healthcare for women
- healthy female
- healthy ladies
- healthy lady
- healthy women
- heavy abnormal bleeding between period
- heavy bleeding after period
- heavy bleeding after period ends
- heavy bleeding between periods
- heavy bleeding during ovulation
- heavy bleeding during period
- heavy bleeding in between periods
- heavy bleeding perimenopause
- heavy bleeding with clots
- heavy blood clots during period
- heavy clotting during period
- heavy flow period
- heavy irregular bleeding between periods
- heavy irregular periods
- heavy menstrual bleeding
- heavy menstrual bleeding causes
- heavy menstrual bleeding with clots
- heavy menstrual discharge
- heavy monthly bleeding
- heavy period after pregnancy
- heavy period blood clots
- heavy period causes
- heavy period clots
- heavy period with clots
- heavy periods
- heavy periods and spotting in between
- heavy periods treatment
- heavy periods with blood clots
- heavy prolonged menstrual bleeding
- heavy spotting
- heavy spotting after period
- heavy spotting between periods
- how to calculate period cycle
- how to count period cycle
- how to get your period
- how to stop heavy periods
- how to stop menstrual bleeding
- how to stop period
- how to stop period bleeding
- how to stop period pain
- how to stop your period early
- i have bleeding between periods
- in between period bleeding
- information on women
- intermenstrual bleeding
- intermittent bleeding between periods
- irregular bleeding
- irregular bleeding after period
- irregular bleeding between periods
- irregular bleeding during period
- irregular heavy bleeding between periods
- irregular heavy periods
- irregular menstruation causes
- irregular period spotting
- irregular periods
- irregular periods and spotting
- irregular periods and spotting in between
- irregular periods causes
- irregular periods symptoms
- irregular spotting
- irregular spotting after period
- irregular spotting between periods
- irregular spotting causes
- keep bleeding after period
- keep spotting after period
- ladies health
- ladies health and fitness
- ladies health care
- ladies health problems
- large blood clots during period
- late period
- light bleeding after menstrual cycle
- light bleeding after menstruation
- light bleeding after period
- light bleeding after period ends
- light bleeding after period finished
- light bleeding after period was over
- light bleeding between periods
- light bleeding in between periods
- light blood after period
- light blood spotting after period
- light menstrual bleeding
- light period
- light spotting after period
- light spotting between periods
- light spotting in between periods
- long heavy period
- long menstrual bleeding
- long menstrual period
- long menstrual period causes
- long menstrual periods
- long period bleeding
- long periods
- long periods menstrual bleeding
- long spotting after period
- men health
- menopause symptoms
- mens health
- menstrual bleeding after period
- menstrual bleeding between periods
- menstrual bleeding for 3 weeks
- menstrual bleeding for a month
- menstrual bleeding in between periods
- menstrual cycle
- menstrual cycle bleeding
- menstrual cycle bleeding between periods
- menstrual cycle phases
- menstrual cycle spotting
- menstrual cycle spotting after period
- menstrual cycle symptoms
- menstrual period
- menstrual period symptoms
- menstrual spotting
- menstrual spotting after period
- menstrual spotting causes
- menstruation
- mild bleeding between periods
- missed period
- monthly period cycle
- more bleeding after period
- my period
- my period is late
- national women's health information center
- no bleeding in periods
- non menstrual bleeding
- normal period cycle
- not bleeding during period
- not bleeding on my period
- occasional bleeding between periods
- older women's health issues
- on and off bleeding after period
- over bleeding after period
- ovulation period
- painful periods
- passing blood clots during period
- period
- period after spotting
- period blood
- period blood clots
- period calculator
- period calendar
- period cramps
- period cramps but no period
- period cycle
- period cycle calculator
- period pain
- period pain but no period
- period problems
- period spotting
- period spotting after period
- period spotting causes
- period symptoms
- period tracker
- periods bleeding
- periods in women
- persistent bleeding between periods
- pms symptoms
- post menstrual cycle bleeding
- post period bleeding
- post period spotting
- pre period symptoms
- prolonged light bleeding after period
- prolonged menstrual bleeding with clots
- prolonged menstrual period
- prolonged period
- pv bleeding
- really heavy period
- really heavy period with clots
- reason of spotting after periods
- reasons for a missed period
- reasons for bleeding after period
- reasons for bleeding between periods
- reasons for irregular periods
- reasons for late period
- reasons for spotting after period
- red blood after period
- red spotting after period
- regular bleeding between periods
- remedy for heavy menstrual bleeding
- s health
- short heavy period
- signs of menstrual cycle
- signs of period
- signs of your period
- slight bleeding after period
- slight bleeding between periods
- slight bleeding in between periods
- small bleeding after period
- small bleeding between periods
- spot bleeding
- spot bleeding after period
- spot bleeding between periods
- spot bleeding in between periods
- spotting a week after period
- spotting after a period
- spotting after a period ends
- spotting after cycle
- spotting after menses
- spotting after menstrual cycle
- spotting after menstrual cycle ends
- spotting after menstrual period
- spotting after menstruation
- spotting after my period
- spotting after period
- spotting after period ends
- spotting after period normal
- spotting after periods causes
- spotting and bleeding
- spotting and discharge after period
- spotting between cycles
- spotting between menstrual cycles
- spotting between periods
- spotting between periods after pregnancy
- spotting between periods causes
- spotting between periods normal
- spotting bleeding after period
- spotting blood
- spotting blood after period
- spotting blood between periods
- spotting during cycle
- spotting during menstruation
- spotting during period
- spotting everyday after period
- spotting for a week after period
- spotting in between cycles
- spotting in between periods
- spotting in between periods causes
- spotting in menstrual cycle
- spotting in menstruation
- spotting in periods
- spotting just after period
- spotting menstrual
- spotting menstrual cycle
- spotting menstrual period
- spotting not period
- spotting period
- spotting periods causes
- spotting week after period
- spotty bleeding between periods
- start bleeding after period
- still bleeding after menstrual cycle
- still bleeding after period
- still slightly bleeding after period
- still spotting after period
- still spotting after period ends
- stomach pain during periods
- stop menstrual bleeding
- stop period bleeding
- super heavy period
- symptoms before period
- symptoms of a period
- symptoms of getting your period
- symptoms of menstrual cycle
- symptoms of period
- symptoms of period coming
- symptoms of spotting after period
- the healthy woman
- topics on women's issues
- treatment for heavy periods
- treatment of heavy menstrual bleeding
- Uncategorized
- unusual bleeding between periods
- unusual menstrual bleeding
- unusual spotting
- unusual spotting between periods
- unusually heavy period
- uterine bleeding between periods
- very heavy period
- very heavy periods
- very light bleeding after period
- very light period
- ways to stop your period
- what can cause abnormal bleeding
- what can cause bleeding between periods
- what can cause bleeding in between periods
- what can cause heavy bleeding between periods
- what can cause irregular bleeding
- what can cause light bleeding between periods
- what can cause spotting between periods
- what can cause spotting in between periods
- what can cause you to bleed after your period
- what causes a heavy period
- what causes a woman to bleed in between periods
- what causes abnormal bleeding between periods
- what causes bleeding after menstruation
- what causes bleeding after period
- what causes bleeding after period ends
- what causes bleeding before your period
- what causes bleeding between periods
- what causes bleeding in between periods
- what causes constant bleeding between periods
- what causes continuous bleeding after period
- what causes heavy bleeding between periods
- what causes heavy menstrual bleeding
- what causes heavy periods
- what causes irregular bleeding between periods
- what causes irregular periods
- what causes irregular periods and spotting
- what causes light bleeding after period
- what causes light bleeding between periods
- what causes light bleeding during periods
- what causes light spotting between periods
- what causes period cramps
- what causes period pains
- what causes period spotting
- what causes spotting
- what causes spotting a week after period
- what causes spotting after a period
- what causes spotting after period
- what causes spotting after period ends
- what causes spotting after your period
- what causes spotting between periods
- what causes spotting during period
- what causes spotting in between periods
- what could cause bleeding after my period
- what could cause bleeding between periods
- what could cause spotting between periods
- what helps period pains
- what is a period
- what would cause a woman to bleed between periods
- what would cause bleeding between periods
- what would cause spotting
- when is my next period
- when is my period due
- why am i spotting
- why are my periods irregular
- why do women have periods
- why is my period early
- why is my period late
- woman bleeding after period
- woman health
- woman s health
- woman spotting between periods
- woman's health insurance
- woman's health services
- womans health
- womans health magazine
- womans magazine
- women
- women & health
- women and health
- women and health issues
- women and healthcare
- women bleeding between periods
- women for health
- women health issues over 50
- women health tips
- women healthy
- women in health
- women information
- women over 50 health issues
- women period
- women period cycle
- women related topics
- women s
- women shealth
- women sites
- women topics
- women website
- women's fitness website
- women's fitness websites
- women's health
- women's health Abilene
- women's health Akron
- women's health Albuquerque
- women's health Alexandria
- women's health Allentown
- women's health Amarillo
- women's health Anaheim
- women's health Anchorage
- women's health and fitness
- women's health and wellness
- women's health Ann Arbor
- women's health Antioch
- women's health Arlington
- women's health articles
- women's health Arvada
- women's health Athens
- women's health Atlanta
- women's health Augusta
- women's health Aurora
- women's health awareness
- women's health Bakersfield
- women's health Baltimore
- women's health Baton Rouge
- women's health Beaumont
- women's health Bellevue
- women's health Berkeley
- women's health Billings
- women's health Birmingham
- women's health Boise
- women's health Boulder
- women's health Bridgeport
- women's health Broken Arrow
- women's health Browning
- women's health Brownsville
- women's health Burbank
- women's health Cambridge
- women's health Cape Coral
- women's health care
- women's health care clinic
- women's health Carlsbad
- women's health Carrollton
- women's health Cary
- women's health Cedar Rapids
- women's health Centennial
- women's health center
- women's health Chandler
- women's health Charleston
- women's health Chattanooga
- women's health Chesapeake
- women's health Chula Vista
- women's health Cincinnati
- women's health Clarksville
- women's health Clearwater
- women's health Cleveland
- women's health clinic
- women's health Colorado Springs
- women's health Columbia
- women's health Columbus
- women's health com
- women's health Concord
- women's health Coral Springs
- women's health Corona
- women's health Corpus Christi
- women's health Costa Mesa
- women's health Cut Bank
- women's health Daly City
- women's health Davenport
- women's health day
- women's health Dayton
- women's health Denton
- women's health Des Moines
- women's health diet
- women's health doctors
- women's health Downey
- women's health Durham
- women's health El Cajon
- women's health El Monte
- women's health Elgin
- women's health Elizabeth
- women's health Elk Grove
- women's health Erie
- women's health Escondido
- women's health Eugene
- women's health Evansville
- women's health Everett
- women's health Fairfield
- women's health Fargo
- women's health Fayetteville
- women's health fitness
- women's health Flint
- women's health Fontana
- women's health Fort Lauderdale
- women's health Fort Wayne
- women's health Fremont
- women's health Fresno
- women's health Frisco
- women's health Fullerton
- women's health Gainesville
- women's health Garden Grove
- women's health Garland
- women's health Gilbert
- women's health Glendale
- women's health Grand Rapids
- women's health Great Falls
- women's health Green Bay
- women's health Greensboro
- women's health Gresham
- women's health Hampton
- women's health Hartford
- women's health Hayward
- women's health Henderson
- women's health Hialeah
- women's health High Point
- women's health Hollywood
- women's health Honolulu
- women's health Huntington Beach
- women's health Huntsville
- women's health Independence
- women's health information
- women's health Inglewood
- women's health insurance
- women's health Irvine
- women's health Irving
- women's health issues list
- women's health issues topics
- women's health Jackson
- women's health Jersey City
- women's health Joliet
- women's health Kalispell
- women's health Kansas City
- women's health Kenosha
- women's health Kent
- women's health Killeen
- women's health Knoxville
- women's health Lafayette
- women's health Lakewood
- women's health Lancaster
- women's health Lansing
- women's health Laredo
- women's health Las Cruces
- women's health Las Vagas
- women's health Lexington
- women's health Lincoln
- women's health Little Rock
- women's health Long Beach
- women's health Louisville
- women's health Lowell
- women's health Lubbock
- women's health Madison
- women's health mag
- women's health magazine
- women's health McAllen
- women's health McKinney
- women's health Mesa
- women's health Mesquite
- women's health Miami
- women's health Miami Gardens
- women's health Midland
- women's health Milwaukee
- women's health Minneapolis
- women's health Miramar
- women's health Mobile
- women's health Modesto
- women's health Montgomery
- women's health Moreno Valley
- women's health Murrieta
- women's health Naperville
- women's health Nashville
- women's health network
- women's health New Haven
- women's health Newark
- women's health Newport News
- women's health Norfolk
- women's health Norman
- women's health North Charleston
- women's health North Las Vegas
- women's health Norwalk
- women's health Oakland
- women's health Oceanside
- women's health Odessa
- women's health Oklahoma
- women's health Olathe
- women's health Omaha
- women's health online
- women's health Ontario
- women's health Orange
- women's health organizations
- women's health Orlando
- women's health Overland Park
- women's health Oxnard
- women's health Palm Bay
- women's health Palmdale
- women's health Pasadena
- women's health Paterson
- women's health Pembroke Pines
- women's health Peoria
- women's health Pittsburgh
- women's health Plano
- women's health Pomona
- women's health Pompano Beach
- women's health Port St. Lucie
- women's health Portland
- women's health problems
- women's health program
- women's health programs
- women's health Providence
- women's health Provo
- women's health Pueblo
- women's health questions
- women's health Raleigh
- women's health Reno
- women's health Rialto
- women's health Richardson
- women's health Richmond
- women's health Riverside
- women's health Rochester
- women's health Rockford
- women's health Roseville
- women's health Round Rock
- women's health Sacramento
- women's health Saint Paul
- women's health Salem
- women's health Salinas
- women's health Salt Lake City
- women's health San Bernardino
- women's health San Buenaventura
- women's health Santa Ana
- women's health Santa Clara
- women's health Santa Clarita
- women's health Santa Maria
- women's health Santa Rosa
- women's health Savannah
- women's health Scottsdale
- women's health services
- women's health Shreveport
- women's health Simi Valley
- women's health Sioux Falls
- women's health site
- women's health South Bend
- women's health Spokane
- women's health Springfield
- women's health St. Louis
- women's health St. Petersburg
- women's health Stamford
- women's health Sterling Heights
- women's health Stockton
- women's health subscription
- women's health Sunnyvale
- women's health Surprise
- women's health Syracuse
- women's health Tacoma
- women's health Tallahassee
- women's health Tampa
- women's health Temecula
- women's health Tempe
- women's health Thornton
- women's health Thousand Oaks
- women's health Toledo
- women's health Topeka
- women's health topics
- women's health Tucson
- women's health Tulsa
- women's health Vallejo
- women's health Vancouver
- women's health Victorville
- women's health Virginia Beach
- women's health Visalia
- women's health Waco
- women's health Warren
- women's health Washington
- women's health Waterbury
- women's health websites
- women's health West Covina
- women's health West Jordan
- women's health West Palm Beach
- women's health West Valley City
- women's health Westminster
- women's health Wilmington
- women's health Winston–Salem
- women's health Worcester
- women's health Yonkers
- women's healthcare center
- women's magazines
- women's medical issues
- women's mental health
- women's websites
- womens health advice
- womens health and fitness magazines
- womens health issues
- womens health magazine subscription
- womens health service
- womens health uk
- womens healthy diet
- womens helth
- womenshealth gov
- womenshealthmag
- womenshealthmag com
- www women
- www women body
- www womenshealth
- www womenshealth gov
- www womenshealthmag com
- young women health
 admin
admin 






